You’re functioning. Handling your responsibilities. But something feels off.
You’re restless, easily irritated, or find yourself overreacting to things that never used to bother you. Maybe your sleep’s off. Or a certain noise, place, or memory pulls you out of the moment, fast.
You’ve probably asked yourself: Is this just stress? Am I anxious all the time? Could it be something deeper, like PTSD?
Knowing the difference between PTSD and anxiety isn’t about slapping on a label.
It’s about finding the right kind of support. Because the strategies that work for one may not work for the other.
We’ll walk through what PTSD and anxiety really feel like, how they overlap, where they diverge, and how to figure out what kind of support fits best, especially for men who don’t always see themselves in the usual mental health playbook.
What Does Anxiety Feel Like (Especially for Men)
Anxiety is your body’s alarm system working overtime. It’s that persistent feeling that something bad might happen, even when things seem fine on the surface.
For many men, it doesn’t show up as panic attacks or tears. Instead, it’s often masked as irritation, overthinking, or tension that doesn’t let up.
You might notice:
- Snapping at small inconveniences
- Mentally rehearsing conversations or worst-case scenarios
- Jaw clenching, muscle tightness, or gut discomfort
- Feeling restless even when you’re supposed to be relaxing
- Trouble falling asleep because your mind won’t slow down
- Throwing yourself into work or workouts just to feel some control
Take Mike, a project manager who appears completely in control at work. No one sees how he rehearses conversations in his head for hours, checks his email dozens of times at night, or feels a constant knot in his stomach. From the outside, he just looks “dedicated” or “intense.” Inside, his nervous system rarely gets a break. |
These patterns aren’t random, they’re part of how anxiety often shows up for men, even if it doesn’t match the usual stereotypes. Anxiety in men can often go unrecognized because of how well it hides behind productivity, irritation, or control.
Common Types of Anxiety
While there are several clinical categories of anxiety, these are the ones most relevant to understanding the difference between PTSD and anxiety:
- Generalized Anxiety Disorder (GAD): This is persistent worry across multiple areas of life, not tied to specific traumatic events. You might worry about work, health, family, or finances, even when things are actually going okay.
- Panic Disorder: This involves sudden, intense episodes of fear that trigger severe physical reactions (panic attacks) when no real danger is present.
- Social Anxiety: Beyond ordinary shyness, this is intense fear of being judged, rejected, or scrutinized in social or performance situations.
What separates anxiety from normal stress is its duration and disruption. Normal stress passes when the situation resolves. Anxiety stays—even when everything looks fine on the outside.
And unlike PTSD, anxiety often doesn’t stem from a specific traumatic event. That difference matters when choosing the right support.
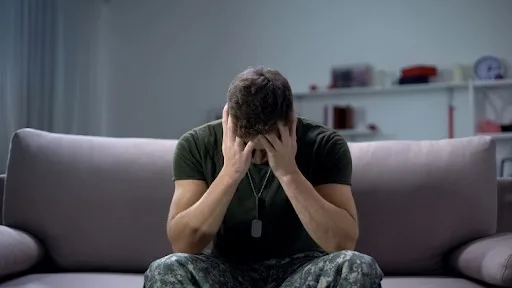
What is PTSD (And How Does It Really Show Up in Men)

Post-Traumatic Stress Disorder (PTSD) develops after experiencing or witnessing a traumatic event.
It’s your brain’s way of trying to protect you from future harm, but the protection system gets stuck in the “on” position.
In men, PTSD often hides in plain sight. It may look like being on edge, getting angry easily, or pulling away from people, not necessarily “looking traumatized.”
Common signs include:
- Constantly scanning your environment, even in safe situations
- Intrusive thoughts, flashbacks, or mental images you didn’t ask for
- Sleep problems, especially nightmares or middle-of-the-night jolts
- Avoiding reminders of what happened (people, places, or topics)
- Feeling emotionally shut down or disconnected
- Jumping at noises or feeling easily startled
- Outbursts of anger or irritability that don’t match the moment
Consider James, a former paramedic who handled countless emergencies with apparent calm. After a particularly difficult call involving a child, he started having nightmares. He found himself avoiding certain neighborhoods and became jumpy at the sound of sirens. To his friends, he just seemed more distant and quick to anger. First responders like James often face cumulative trauma that builds slowly until it overwhelms the body’s ability to cope. |
Complex PTSD vs Single-Event Trauma
Single-Event PTSD typically develops after a clearly defined traumatic incident (accident, assault, natural disaster, combat experience).
Complex PTSD (C-PTSD), on the other hand, forms in response to prolonged or repeated trauma, often occurring in situations where escape was difficult or impossible.
This might include childhood abuse, domestic violence, or long-term exposure to war.
Complex PTSD includes the core symptoms of PTSD plus additional challenges with emotional regulation, negative self-perception, and difficulty in relationships.
Both forms of PTSD can significantly impact your day-to-day life, even if you’ve become skilled at hiding the symptoms from others.
PTSD vs Anxiety: How They’re Similar and How They’re Different
PTSD and anxiety often look similar on the surface. Both can make everyday situations feel harder than they should.
But they stem from different places and need different kinds of support. Understanding how they overlap, and where they diverge, can help you figure out what fits your experience.
Shared Symptoms of PTSD and Anxiety
PTSD and anxiety can both affect your body, mind, and relationships in ways that aren’t always obvious to others.
You might notice:
- Feeling tense, jumpy, or constantly on edge
- Trouble falling asleep or staying asleep
- Difficulty focusing or following through
- Physical symptoms like clenched muscles, headaches, or digestive discomfort
- Avoiding certain situations just to feel “okay”
- Work or relationships suffering because you’re emotionally checked out or irritable
- Regular situations feeling overwhelming or hard to handle
This overlap explains why it can be confusing to determine what’s happening, especially if you’re trying to figure it out on your own.
Difference Between PTSD and Anxiety Symptoms
Where these conditions differ is often in how they started, how they show up, and what triggers them. Recognizing these patterns can help guide the kind of support you seek.
Root Cause:
- PTSD usually follows a traumatic experience—something your nervous system registered as deeply threatening.
- Anxiety might build over time, often without one specific trigger. It can come from stress, health factors, or patterns learned early in life.
Thought Patterns:
- PTSD often brings flashbacks or intrusive memories, scenes you didn’t choose to revisit.
- Anxiety tends to revolve around “what ifs,” worst-case scenarios, and anticipating danger.
Nervous System Response:
- PTSD can create a rollercoaster of feeling hyper-alert one moment, and emotionally shut down the next.
- Anxiety keeps your body in a constant “fight or flight” state: tense, wired, and hard to calm.
Triggers:
- PTSD tends to be reactive, set off by sights, sounds, or memories tied to trauma.
- Anxiety is more anticipatory, rooted in fear of what might happen, even without a clear cause.
Timeline:
- PTSD symptoms typically begin after a traumatic event.
- Anxiety symptoms may develop gradually and stick around even in the absence of a crisis.
These distinctions matter because they affect which treatment approaches will be most effective.
How Trauma Plays a Role in Both ConditionsTrauma can be the root cause of PTSD and a contributing factor to anxiety disorders. And for many men, the line between the two isn’t always clear—especially when symptoms start overlapping. Research Trauma can lead to a hyperactive amygdala (your brain’s internal alarm system) and reduced activity in the prefrontal cortex, the part that helps regulate fear and stress. When that regulation weakens, it becomes harder to calm down after being triggered or to distinguish between real danger and perceived threat. This is why some men experience flashbacks tied to a specific event, while others feel a constant sense of unease with no clear source. And it’s also why both experiences may include racing thoughts, sleep disruption, or physical tension. The key takeaway? PTSD and anxiety don’t always exist in isolation. For many men, they show up together, and both are treatable with the right support. |
How to Tell if You Have Anxiety, PTSD, or Both
While only a qualified professional can provide an official diagnosis, these insights may help you better understand your experience.
Signs That Point to Anxiety
- Worry spans multiple areas of life—work, health, relationships, even when things seem stable
- The anxiety isn’t clearly tied to a traumatic event
- You anticipate worst-case scenarios often, even in new or low-risk situations
- Symptoms like muscle tension, racing thoughts, or restlessness show up across different settings
- Sleep problems or trouble relaxing persist without an obvious trigger
Signs That Point to PTSD
- Your symptoms began after a specific traumatic event, like an accident, assault, or loss
- You experience flashbacks, intrusive thoughts, or nightmares tied to that event
- You avoid reminders of the trauma, even subtly, like skipping certain routes or conversations
- You feel emotionally disconnected from others or flat inside
- Triggers cause intense physical or emotional reactions that feel disproportionate to the moment
Recognizing Comorbidity (Having Both)
- Your symptoms began after a specific traumatic event, like an accident, assault, or loss
- You experience flashbacks, intrusive thoughts, or nightmares tied to that event
- You avoid reminders of the trauma, even subtly, like skipping certain routes or conversations
- You feel emotionally disconnected from others or flat inside
- Triggers cause intense physical or emotional reactions that feel disproportionate to the moment
Remember that these categories aren’t rigid, many people experience symptoms that don’t fit neatly into one box.
What matters most is finding support that addresses your specific experience.
Diagnosis and Treatment for PTSD and Anxiety
Getting the right diagnosis isn’t about putting a label on you—it’s about understanding your experience well enough to know what actually helps. Anxiety and PTSD can look similar, but they often need different kinds of support.
Professional Assessment
A thorough assessment by a licensed therapist typically includes:
- Discussion of current symptoms and their impact on your life
- Exploration of personal and family history
- Evaluation of any traumatic experiences
- Screening questionnaires to assess symptom patterns
- Consideration of other factors like substance use or medical conditions
This process isn’t about labeling you, it’s about understanding your unique experience to create an effective treatment plan.
Evidence-Based Treatment Approaches
While treatment is always tailored to individual needs, these approaches have strong research support:
For Anxiety:
- Cognitive Behavioral Therapy (CBT) helps you identify and change thought patterns that fuel anxiety
- Mindfulness-based techniques improve your ability to stay present rather than getting caught in worry cycles
- Exposure therapy gradually helps you face feared situations in a controlled way
- Certain medications can help manage symptoms while you work on long-term strategies
For PTSD:
- Eye Movement Desensitization and Reprocessing (EMDR) helps process traumatic memories without having to discuss them in detail
- Trauma-Focused CBT addresses both the emotional and cognitive aspects of trauma
- Prolonged Exposure therapy helps reduce avoidance behaviors
- Medications may help manage specific symptoms like sleep disturbances or extreme hypervigilance. Some may even benefit from newer interventions, like ketamine-assisted therapy, which has shown promise in treatment-resistant PTSD when used alongside trauma-focused approaches.
For Both Conditions:
- Approaches that address nervous system regulation
- Physical activity and body-based interventions
- Structured stress management techniques
- Building a supportive social network
The most effective treatment plans often combine several approaches, adjusted based on your response and needs.
Why Seeking Help is Important
Living with untreated anxiety or PTSD takes a significant toll. Beyond the immediate discomfort, these conditions can affect:
- Your physical health (through chronic stress)
- Your relationships with partners, family, and friends
- Your work performance and career trajectory
- Your ability to engage in activities you once enjoyed
- Your overall quality of life
The good news is that these conditions respond well to proper treatment. With the right support, many men experience substantial relief and return to living more fulfilling lives.
How Denver Men’s Therapy Can Help

If you’re dealing with anxiety or trauma, therapy doesn’t need to feel vague or aimless.
At Denver Men’s Therapy, we offer structure, clarity, and real tools, delivered in a way that respects how men process things.
Here’s what makes our approach work:
- Specialized support: Our licensed therapists have advanced training in treating anxiety, trauma, and PTSD in men using evidence-based approaches.
- Therapy built for men: We don’t assume you want to sit and talk endlessly. We focus on what helps: practical tools, clear feedback, and space to work things through at your pace.
- Structured, not rigid: We start with a focused assessment, then develop a plan that fits your goals, not a one-size-fits-all model.
- Respect for your process: Some things are hard to talk about. That’s why our sessions are confidential, grounded, and never pushy.
- Results that matter: We aim to reduce overwhelm, improve emotional regulation, and help you regain control, in relationships, work, and within yourself.
We draw from a range of effective options, including:
- EMDR therapy for trauma that’s hard to move past
- CBT and integrative techniques that help manage anxiety patterns
- Mind-body strategies to regulate nervous system overwhelm
You don’t have to figure it out alone. Our approach meets you where you are—and moves at your pace.
Related read: What therapy is actually like for men
Finding the Right Support Starts Here
Knowing whether you’re dealing with anxiety, PTSD, or both is a powerful first move. Here’s how to begin:
- Reflect on your symptoms: Consider which patterns described in this article match your experience.
- Reach out for a consultation: Schedule a confidential consultation with Denver Men’s Therapy to talk it through in a private, judgment-free setting.
- Begin the process: Work with your therapist to develop a clear plan that addresses your unique needs and goals.
For men looking to build healthier coping tools even beyond therapy, it helps to start with small habits that protect emotional resilience. This guide on how to improve men’s mental health offers simple ways to build momentum.
Support isn’t about fixing something broken. It’s about working with someone who sees the full picture and can help you move through it. You don’t have to carry this alone.
FAQs
What is the difference between PTSD and panic disorder?
While both involve intense anxiety, they differ in key ways. Panic disorder involves recurring panic attacks that come on suddenly without clear triggers. PTSD involves a broader range of symptoms (including flashbacks, avoidance, and hypervigilance) specifically tied to past trauma.
Panic attacks can occur within PTSD, but they’re typically triggered by trauma reminders rather than happening randomly.
Can you have both complex PTSD and generalized anxiety disorder at the same time?
Yes, you can have both conditions simultaneously.
Complex PTSD develops from prolonged trauma and includes symptoms beyond standard PTSD, such as difficulties with emotional regulation and self-perception. Generalized Anxiety Disorder involves persistent worry across multiple life areas.
These conditions can co-exist, with each requiring specific treatment components for full recovery.
How can I support a loved one struggling with PTSD or Anxiety?
Supporting someone with PTSD or anxiety involves several key approaches:
- Learn about the condition to better understand their experience
- Be patient and non-judgmental about their symptoms and triggers
- Avoid pressuring them to talk about trauma or face feared situations
- Encourage professional support from specialists in trauma and anxiety
- Ask how you can help rather than assuming you know what they need
- Take care of yourself too, as supporting someone with these conditions can be challenging
Professional guidance can help both of you navigate this journey effectively.